What You Should Know About Fetal Echocardiogram
Congenital heart diseases (CHDs) are the most common congenital anomalies with reported incidence of up to 75 per 1000 live births. Approximately half or more of the CHDs are minor and are easily corrected by surgery; however, the remainder accounting for over half of the deaths from congenital abnormalities in childhood. The reported incidence of moderate to severe malformations is 6 to 8 in 1000 live births (19/1000 live births if serious bicuspid aortic valve is included).
Over the past decade, the prevalence of prenatally diagnosed congenital heart disease (CHD) has risen, mostly due to improved obstetric screening. Fetal echocardiography is broadly defined as a detailed sonographic evaluation that is used to identify and characterize fetal cardiac anomalies prior to delivery. Prenatal diagnosis of CHD is considered beneficial for the neonate, allowing for the immediate delivery of medical care and decreasing morbidity associated with delayed diagnosis. Carnegie Imaging for Women is excited to announce that we are one of the few maternal fetal medicine imaging centers offering screening fetal echocardiogram service for patients. If a cardiac anomaly is suspected on our screening echocardiogram we can facilitate timely evaluation by the pediatric cardiologist.
What’s the difference between cardiac views on detailed anatomy compared to fetal echocardiogram?
This specialized diagnostic procedure is an extension of the basic fetal cardiac screening performed with the detailed anatomy surveillance, which typically only includes the 4-chamber heart view and outflow tracts. The fetal echocardiogram is a detailed evaluation of cardiac structure which involves a sequential segmental analysis of the 3 basic areas that include the atria, ventricles, and great arteries with their connections.
| Cardiac views on standard detailed anatomy | Cardiac views on fetal echocardiogram |
|
|
What cannot be diagnosed on screening fetal echocardiogram?
Screening fetal echocardiogram can identify approximately 80% of all congenital heart defects; however, fetal echocardiogram cannot rule out the presence of small septal defects, mild valvar abnormalities, coronary artery anomalies, or partial anomalous pulmonary venous return. Additionally, a fetal echocardiogram cannot predict the postnatal outcome of patent ductus arteriosus, patent foramen ovale, or the development of coarctation upon ductal closure.
When should patient have a screening fetal echocardiogram?
Therefore, we recommend that all patients who have indications for a fetal echocardiogram obtain one in the antenatal period. Typically screening fetal echocardiograms are performed between 20 to 22 weeks of gestation and can be performed at the same date as her scheduled detailed anatomical surveillance. Technical limitation, such as maternal obesity, fetal prone position, and late gestation, can make a detailed cardiac evaluation difficult due to acoustic shadowing and a repeat examination at a different time may be necessary.
Who should have a screening fetal echocardiogram?
Indications for fetal echocardiography are based on a variety of parental and fetal risk factors for CHDs. Common indications for referral to Carnegie Imaging for Women for fetal echocardiogram include
| Fetal Indications | Maternal Indications |
|
|
Figure 1: Using 4D (STIC) color Doppler to demonstrate normal crossing of the outflow tracts.

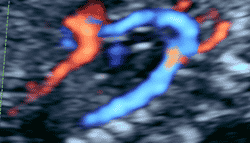
Figure 2: Demonstration of muscular VSD using color Doppler while septum appeared intact on gray scale
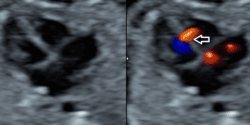
Figure 3: 4D power Doppler of normal ductal arch

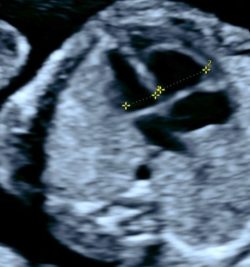
Figure 4: 3 vessel trachea view demonstrating right sided aortic arch with vascular ring around trachea
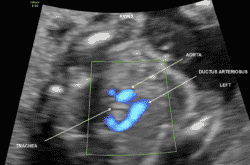
Figure 5: Coarctation of aorta diagnosed at 20 week screening fetal echo (referral reason: SSRI use)
- Discrepancy of ventricle size
- Discrepancy of vessel size on 3 VVT
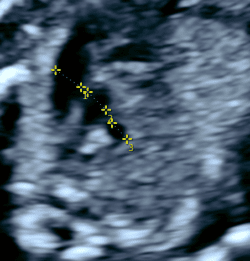
- Constriction of the aortic arch
- Turbulent flow seen at the level of constriction
Carnegie Imaging for Women blogs are intended for educational purposes only and do not replace certified professional care. Medical conditions vary and change frequently. Please ask your doctor any questions you may have regarding your condition to receive a proper diagnosis or risk analysis. Thank you!










 Contact Us
Contact Us







 Contact Us
Contact Us Carnegie South
Carnegie South


