3D Coronal Plane of the Uterus for IUD Placement: A Game Changer
Over the last decade, there has been a resurgence in the popularity of long-acting reversible contraceptives (LARCS) among reproductive age women. Amongst the LARCS, the intrauterine contraceptive device (IUD) is the most commonly used. The two kinds of IUDs that are most frequently used are the copper-containing devices (e.g ParaGard, Copper T-380A) and the hormone-releasing IUDs (e.g Mirena, Skyla, Kyleena and Liletta). These two types of IUD are T-shaped.
The majority of women are pleased with their IUDs and continuation rates have been estimated at about 80%. After placement, changes in menstrual flow may occur. Copper-containing devices are more commonly associated with bleeding and dysmenorrhea; while hormone-releasing IUDs which contain progesterone are more often associated with amenorrhea.
Abnormal bleeding, pelvic pain, or inability to feel the strings is a common indication for a pelvic ultrasound.
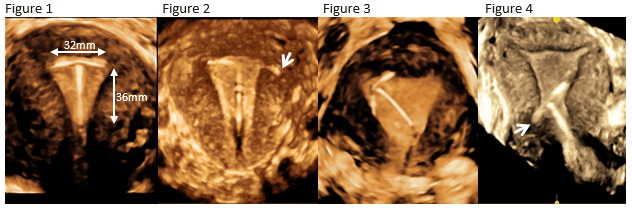
Conventional transabdominal and transvaginal sonography can identify the presence of the IUD within the uterus. However, for more precise localization of the IUD, three-dimensional (3D) sonography is essential. 3D transvaginal sonography demonstrates the coronal view of the uterus, which results in a clear and a more precise localization of the IUD within the uterine cavity. (Figure 1 normally placed IUD). The strings are attached to an inferior portion of the shaft and at times can be sonographically identified. The ParaGard, Mirena, and Liletta measure 32 mm across the arms and have a shaft length of 36 mm and 32 mm, respectively. The Skyla and Kyleena are smaller, measuring 28 mm across the arms and have a shaft length of 30mm. Mirena was approved to be used in parous women, while the others are approved for all women. The Skyla with its smaller arms span makes it a better option for nulliparous women.
Uterine size may differ among women (e.g. parous vs. nulliparous); therefore, assessing the transverse fundal diameter pre-insertion using the 3D coronal plane allows placement of the correct size IUD (Figure 1).
- Different types of malpositioned IUDs can be diagnosed by the 3D coronal view.
- In embedment there is penetration of the IUD into the myometrium without extension through the serosa (Figure 2 – embedment of an arm (arrow).
- In displacement, there can be rotation (Figure 3 rotated IUD) or inferior positioning of the IUD in the lower uterine segment or cervix (Figure 4- Inferior displacement with embedment of one of the arms (arrow)).
- Perforation can be partial or complete with penetration of the IUD through the serosa.
- Lastly, fragmentation in which there is retention of a broken piece of the IUD after expulsion or removal.
- Pre- insertion 3D ultrasound in nullipara can assure that the correct sized IUD will be placed by matching the arm length of the IUD with the transverse fundal uterine diameter.
- Post-insertion IUD localization in ALL patients using the 3D coronal plane assures correct placement.
Reference: Shipp TD and Bromley B. IUD issues: Zero in with ultrasound. Contemporary OB/GYN, 2016
Carnegie Imaging for Women blogs are intended for educational purposes only and do not replace certified professional care. Medical conditions vary and change frequently. Please ask your doctor any questions you may have regarding your condition to receive a proper diagnosis or risk analysis. Thank you!










 Contact Us
Contact Us







 Contact Us
Contact Us Carnegie South
Carnegie South


